Image Source: trumedsystems.com
How Long Can A Vaccine Be Out Of The Fridge: A Guide
So, how long can a vaccine stay out of the fridge? It’s a crucial question. The simple answer is, it really depends. Each vaccine has its own specific rules. These rules tell you how long it can be safely kept at room temperature. If a vaccine is left out too long or gets too hot or too cold, it might stop working right. This means it loses its power to protect you or others from disease. Proper storage is key to making sure vaccines do their job.
This guide will help you learn why keeping vaccines at the right temperature is so important. We will look at what happens when they get too warm or too cold. You will also learn about the rules for keeping vaccines safe and effective.
Grasping Vaccine Stability
Vaccines are like little helpers that teach your body how to fight off germs. They are made of delicate parts. These parts can be easily harmed by heat, cold, or light. Keeping vaccines at the correct temperature helps these helpers stay strong and ready to work.
Vaccine stability means how well a vaccine holds up over time. It means it keeps its ability to protect you. If a vaccine is not stored correctly, its stability can be ruined. It might not work anymore.
Think of a carton of milk. You know milk needs to stay cold in the fridge. If you leave milk out on the counter for a long time, it goes bad. It’s not safe to drink. Vaccines are similar. They need special care with temperature to stay good and safe.
The Cold Chain: What It Is and Why It’s Vital
Keeping vaccines at the right temperature from the moment they are made until they are given is called the cold chain. It is a system that ensures vaccines are always stored within their recommended storage guidelines.
The cold chain starts at the factory. Vaccines are made there. They are then stored in big fridges or freezers. When they are shipped, they travel in special containers. These containers keep the temperature just right. They go to hospitals, clinics, and pharmacies. These places also have special fridges and freezers for vaccines.
- Factory storage: Big, controlled rooms.
- Shipping: Special cold boxes.
- Clinic storage: Dedicated vaccine fridges or freezers.
- Handling before use: Kept cool until given.
Every step in this journey is important. If the temperature is wrong at just one step, the vaccine can be damaged. This breaks the cold chain requirements. A broken cold chain means the vaccine might not work.
Cold chain requirements are the strict rules for keeping vaccines at the right temperature. These rules include:
- Storing vaccines in approved fridges or freezers.
- Using temperature monitors to check the temperature all the time.
- Keeping detailed records of the temperature checks.
- Having a plan for what to do if the power goes out or the temperature goes wrong.
Following these rules is not just a suggestion. It is necessary to make sure vaccines stay effective.
Recommended Storage Guidelines
Each vaccine comes with specific instructions from the company that made it. These instructions tell you the vaccine storage temperature. Most vaccines need to be kept in a fridge. The usual temperature range for vaccine fridges is between 2°C and 8°C (36°F and 46°F). Some vaccines need to be frozen. They need temperatures as low as -15°C (5°F) or even colder.
These temperatures are not chosen by chance. They are found through lots of testing. Tests show what temperature keeps the vaccine stable and working for the longest time.
- Fridge Temps: Usually 2°C to 8°C (36°F to 46°F). This is like your home fridge but needs to be very stable.
- Freezer Temps: Can be -15°C (5°F) or much colder, depending on the vaccine.
Storing vaccines outside these ranges is called a temperature excursion. This is a big problem. It can harm the vaccine.
Clinics and hospitals use special vaccine fridges. These fridges are different from home fridges. They are better at keeping a steady temperature. They often have alarms that go off if the temperature goes too high or too low. They also have devices that record the temperature constantly. This helps track any temperature excursion.
What Happens When It’s Out of the Fridge?
When a vaccine is taken out of its proper cold storage, it starts to warm up. If it warms up too much, it can lose its vaccine potency. This means it becomes less effective. It might not give the person who gets the shot the full protection they need.
Room temperature vaccine exposure happens when a vaccine is left out in a place that is not kept cool. The air temperature in the room is usually much higher than the needed storage temperature.
The effect of room temperature vaccine exposure depends on several things:
- How hot is the room? A very hot room will harm the vaccine faster than a cool room.
- How long is it out? Even a short time can be bad for some vaccines. Longer times are usually worse.
- What type of vaccine is it? Some vaccines are more sensitive to heat than others.
- Was it exposed to light? Some vaccines are also damaged by light.
When a vaccine gets too warm, the delicate parts inside can break down. They change shape. They can’t do their job of training your body’s defenses anymore. This is an example of improper storage effects. The vaccine might look okay, but it is no longer able to provide protection.
A temperature excursion is any time a vaccine is stored outside its correct temperature range. This can be too hot or too cold (freezing). Freezing can be just as bad, or even worse, than getting too hot for some vaccines. For example, freezing can break down the liquid part of some vaccines, ruining them completely.
Deciphering How Long is Too Long
There is no single answer for how long a vaccine can be out of the fridge. It is different for almost every vaccine. The recommended storage guidelines for each specific vaccine will tell you.
Some vaccines must be given almost immediately after being taken from the fridge. They might only be stable at room temperature for a very short time, maybe just a few minutes. Others might be able to stay at room temperature for a few hours. A few special vaccines can last longer outside the fridge, but this is not common.
You must check the information for the specific vaccine you are using. This information is usually on the vaccine box or in the paper insert that comes with it. It will state the allowed room temperature vaccine exposure time and temperature range.
Here is a simplified idea (remember, check the actual vaccine data!):
| Vaccine Type (Example) | Usual Storage Temp | Max Time Out of Fridge (Example) | Allowed Temp When Out (Example) |
|---|---|---|---|
| Type A | 2°C to 8°C | 2 hours | Up to 25°C |
| Type B | 2°C to 8°C | 12 hours | Up to 25°C |
| Type C | -15°C or colder | Must be used right after thawing | N/A |
Disclaimer: The above table uses example data only. Always refer to the manufacturer’s specific product information for real vaccines.
If a vaccine is left out longer than the time allowed or gets hotter than the allowed temperature, it has had a temperature excursion. Even if it was only slightly outside the limits, it could be damaged. The vaccine potency might be reduced. It might not work right.
Factors Affecting Stability Outside the Fridge
Several things can make a vaccine lose its power faster when it is out of the fridge. These factors relate directly to vaccine stability.
- Temperature: This is the most important factor. Higher temperatures cause the vaccine parts to break down faster. Even if the room temperature is within the allowed range, direct sunlight can heat the vaccine vial quickly.
- Light: Some vaccines are sensitive to light. Exposure to bright room lights or sunlight can damage them. This is why many vaccines come in dark vials or boxes. They need to be protected from light even when they are in the fridge or out for a short time during vaccine handling.
- Vibration: While less common as a major issue during short room temperature vaccine exposure, constant shaking can also potentially affect the delicate parts of some vaccines over time. This is more of a concern during transport.
- Time: The longer a vaccine is outside its recommended temperature range, the higher the chance it will be damaged. The harm is cumulative. Short excursions are less likely to cause damage than long ones, but any excursion carries a risk.
Protecting vaccines from these factors during vaccine handling is crucial. This means keeping them covered if they are light-sensitive and minimizing the time they are out of controlled temperature.
Proper Vaccine Handling
Good vaccine handling is key to keeping vaccines safe and effective. This goes beyond just storage temperature. It includes how you move, prepare, and give the vaccine.
- Plan Ahead: Take vaccines out of the fridge only when you are ready to use them. Take out only what you need for the next short period.
- Be Quick: Give the vaccine as soon as possible after taking it out. Minimize room temperature vaccine exposure time.
- Protect from Light: If the vaccine is sensitive to light, keep it in its box or a dark place until you are ready to draw it up.
- Don’t Refreeze: If a vaccine that should be refrigerated accidentally freezes, you usually cannot use it. Do not try to thaw it and put it back in the fridge or freezer.
- Monitor Temperature: Always use temperature monitoring devices in your vaccine storage units. Check them regularly.
- Record Keeping: Keep clear records of vaccine stock, where they are stored, and temperature checks. Note any temperature excursion.
Even for vaccines that can be at room temperature for a short time, best practice is to keep them in the fridge until the moment they are needed. This helps ensure vaccine viability and vaccine potency.
Interpreting Improper Storage Effects
What happens if a vaccine has been stored improperly? The main risk is that it loses its vaccine potency. This means it won’t protect the person who gets it as well as it should. The vaccine might look normal. You often cannot tell just by looking at it if it has been damaged by temperature.
Sometimes, improper storage, like freezing, can cause visible changes. For example, the liquid might look cloudy or have tiny bits in it. This is a sign of improper storage effects. However, a vaccine damaged by heat often looks exactly the same as a good vaccine. This is why relying on temperature monitoring and records is so important.
Using a vaccine that has lost potency is not just wasteful. It leaves the person unprotected. They think they are safe, but they are not. This is a serious public health issue.
Signs that might point to improper storage effects (but remember, often there are no visible signs):
- Cloudiness or discoloration in a vaccine that should be clear.
- Particles floating in the liquid.
- If a freeze-sensitive vaccine looks like it has separated or cracked (like milk that has frozen and thawed).
- Damaged packaging that suggests mishandling.
If you suspect a vaccine might have been stored improperly, do not use it.
What to Do After a Temperature Excursion
A temperature excursion means a vaccine has been stored outside its recommended temperature range. This is a serious event in vaccine handling.
If you discover a temperature excursion, you must act fast.
- Isolate the Vaccine: Immediately move the affected vaccines to a safe place. Clearly label them “DO NOT USE” or “QUARANTINED”. This stops anyone from accidentally using them.
- Check the Temperature: Find out exactly how hot or cold the storage unit got and for how long. Use your temperature monitoring device records.
- Consult Guidelines: Refer to the specific vaccine’s manufacturer guidelines or your local health authority’s protocols. These documents will tell you if the vaccine might still be usable after a specific type of excursion. Some vaccines have data on stability at different temperatures for limited times.
- Contact Experts: If the guidelines are not clear, or if it’s a significant excursion, contact the vaccine manufacturer or your local health department. They have experts who can help decide if the vaccine is still good based on the specific temperature data and the vaccine type.
- Document Everything: Write down exactly what happened, when it happened, how long it lasted, the temperatures recorded, and what you did about it. This is very important for tracking and reporting.
- Dispose of Compromised Vaccines: If the decision is made that the vaccines are no longer viable, they must be disposed of properly. Do not return them to regular stock.
Never assume a vaccine is okay after a temperature excursion. The risk of using a vaccine that doesn’t work is too high. The goal is to protect people, and that requires using vaccines that are known to be effective. Following these steps protects the vaccine viability and ensures people get working vaccines.
Why You Shouldn’t Guess
Guessing if a vaccine is still good after it has been out of the fridge is risky. As mentioned, you usually cannot see if a vaccine has lost its vaccine potency. It might look perfectly fine.
If you use a vaccine that is no longer potent, the person vaccinated is not protected. This can have serious effects:
- False Sense of Security: The person thinks they are immune but are not. They might take risks they wouldn’t otherwise.
- Continued Spread of Disease: An unprotected person can still catch and spread the disease.
- Wasted Resources: The vaccine dose is wasted, and the effort of giving the shot is wasted.
- Loss of Trust: If people find out they received ineffective vaccines, trust in vaccination programs can be damaged.
Ensuring vaccine viability means strictly following recommended storage guidelines and cold chain requirements. It means being careful with vaccine handling. If there is any doubt because of room temperature vaccine exposure or a temperature excursion, it is always safer not to use the vaccine.
The cost of replacing a few potentially damaged vaccine doses is far less than the cost to individual health and public trust if ineffective vaccines are used.
Concrete Steps for Safe Vaccine Handling
To ensure vaccines stay effective, everyone involved in vaccine handling must follow strict rules. This includes doctors, nurses, pharmacists, and anyone who stores or moves vaccines.
- Check Deliveries: When vaccines arrive, check the packaging. Make sure cold chain monitors inside the box show the temperature stayed correct during shipping. Put the vaccines away in the right storage unit immediately.
- Use Proper Equipment: Only use vaccine-approved refrigerators or freezers. Do not use regular household fridges, as their temperature can vary too much. Use digital temperature monitors with alarms and recording capabilities.
- Place Correctly in Storage: Do not store vaccines in the doors of the fridge or freezer. The temperature in the door changes too much when it is opened and closed. Store them in the middle of the unit. Do not pack the unit too full; air needs to circulate.
- Limit Time Out: Only remove vaccine vials from the fridge or freezer right before you are going to use them. Prepare one dose at a time if possible.
- Protect from Light: Keep vaccines in their original boxes until ready to draw up the dose, especially if they are light-sensitive.
- Check Expiry Dates: Rotate stock so that vaccines expiring sooner are used first.
- Train Staff: Make sure everyone who handles vaccines knows the rules and procedures. Regular training is important.
These steps help maintain the cold chain requirements and protect vaccine stability, ensuring vaccine potency and vaccine viability.
Reviewing Specific Vaccine Examples (General)
It’s hard to give exact times for every vaccine because guidelines change and differ. But knowing that different vaccines have different tolerances is important. This is why you cannot apply the rule for one vaccine to another.
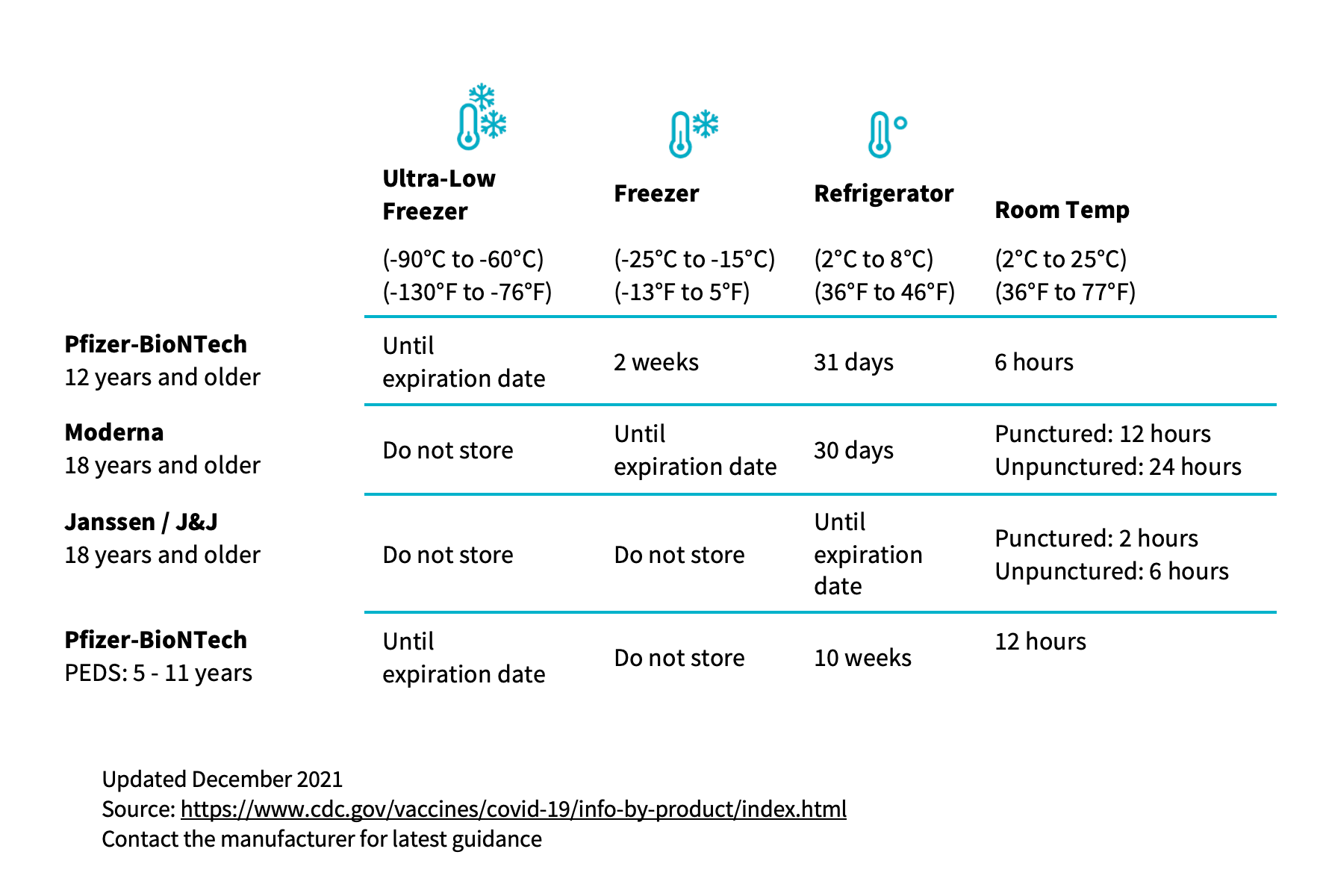
- Some mRNA Vaccines: These often need very cold freezer storage (-20°C or even -80°C). Once thawed and put in the fridge, they have a limited shelf life (e.g., 30 days). Once taken out of the fridge and prepared for use, they might only be good for a few hours at room temperature. This shows how specific the rules are.
- Many Routine Vaccines (like Measles, Mumps, Rubella – MMR): These typically need standard fridge temperatures (2°C to 8°C). They might have a limited time they can spend at room temperature, perhaps a few hours, before they must be discarded.
- Oral Vaccines: Some vaccines given by mouth might have different storage needs than injected ones. Always check the specific product.
These examples show why looking up the specific recommended storage guidelines for each vaccine product is absolutely necessary. A guess based on another vaccine could ruin the dose.
Key Takeaways on Temperature and Time
To recap the important points about how long a vaccine can be out of the fridge:
- It varies greatly. There is no one-size-fits-all answer.
- Each vaccine has specific rules. Check the manufacturer’s information or label.
- Time and Temperature Matter. Being out too long or getting too hot (or too cold, if it’s freeze-sensitive) damages vaccines.
- Damage is often Invisible. A vaccine can look fine but not work if stored improperly.
- Cold Chain is Critical. The system of keeping vaccines cold from factory to patient is vital.
- Temperature Excursions are Serious. Any time the temperature is wrong, the vaccine is at risk.
- Do Not Guess. If you think a vaccine might have been damaged by temperature, do not use it. Consult experts.
Following strict vaccine storage temperature rules, respecting cold chain requirements, and using careful vaccine handling practices are the only ways to be sure vaccines will work and provide the protection people need. Protecting vaccine stability is protecting public health.
Frequently Asked Questions
Q: Can I store vaccines in my home fridge?
A: No, not for medical use. Home fridges do not keep a steady temperature. They can get too warm or too cold, especially in the door. Proper vaccine fridges are needed to meet strict vaccine storage temperature rules.
Q: What happens if a vaccine freezes?
A: Many vaccines are damaged by freezing. The liquid part can expand and break down the vaccine parts. If a vaccine that should be refrigerated freezes, you usually must throw it away. Do not try to use it. Freezing is a type of temperature excursion.
Q: How long can I keep a vaccine out of the fridge while preparing it?
A: This time should be as short as possible. Check the specific vaccine’s instructions. Some say use immediately after taking from the fridge. Others might allow a few minutes or hours. This is part of vaccine handling.
Q: How do I know if my vaccine fridge is working right?
A: Use a special temperature monitoring device made for vaccine storage. These devices record the temperature constantly and should have alarms. Check the readings regularly. This helps you spot a temperature excursion quickly.
Q: If a vaccine was left out too long but looks fine, can I still use it?
A: No. Improper storage effects, like losing vaccine potency, are often not visible. Using a vaccine after a known temperature excursion or too much room temperature vaccine exposure is risky. The person might not get protected. Always follow the rules or consult experts.
Q: Where can I find the specific storage rules for a vaccine?
A: Look at the vaccine’s packaging or the paper insert that comes with it. This has the recommended storage guidelines from the manufacturer. You can also find this information on the manufacturer’s website or through health authority resources.
Q: What is the difference between vaccine potency and viability?
A: Vaccine potency means the vaccine has enough active parts to work and cause an immune response. Vaccine viability is similar, often used for live vaccines, meaning the live part is still alive and active. Both mean the vaccine is able to do its job. Improper storage harms both potency and viability.
Following the rules for vaccine storage temperature, respecting cold chain requirements, and being careful with vaccine handling are essential steps. They protect vaccine stability and ensure that vaccines work the way they are supposed to. This keeps communities safe.
